Challenges in preventative cardiology – is no-code the solution?
Cardiovascular diseases (CVD) are the most common cause of death in the world, despite being categorized as preventable illness.
The epidemic of CVD disproportionately affects different countries, with 80% of deaths occurring in low-income and middle-income countries. (1)

Cardiovascular diseases (CVD) are the most common cause of death in the world, despite being categorized as preventable illness. The epidemic of CVD disproportionately affects different countries, with 80% of deaths occurring in low-income and middle-income countries. (1)
There are multiple factors contributing to development of CVD – ranging from biological factors to public health risks. Due to a rapid development of health technology in the recent years, solutions to the issues faced by health care providers have become solvable.
Biological risk factors
After decades of research, health care community has developed a clear understanding of biological risk factors that can contribute to CVD. These risk factors can be divided into modifiable and non-modifiable risk factors. (2) Modifiable risk factors can successfully be controlled by medical interventions. (3)
Modifiable risk factors:
• High blood pressure
• Smoking
• Diabetes
• Physical inactivity
• Obesity
• High blood cholesterol
Non-modifiable risk factors:
• Age
• Gender
• Genetic factors
• Race and ethnicity
How no-code can assist
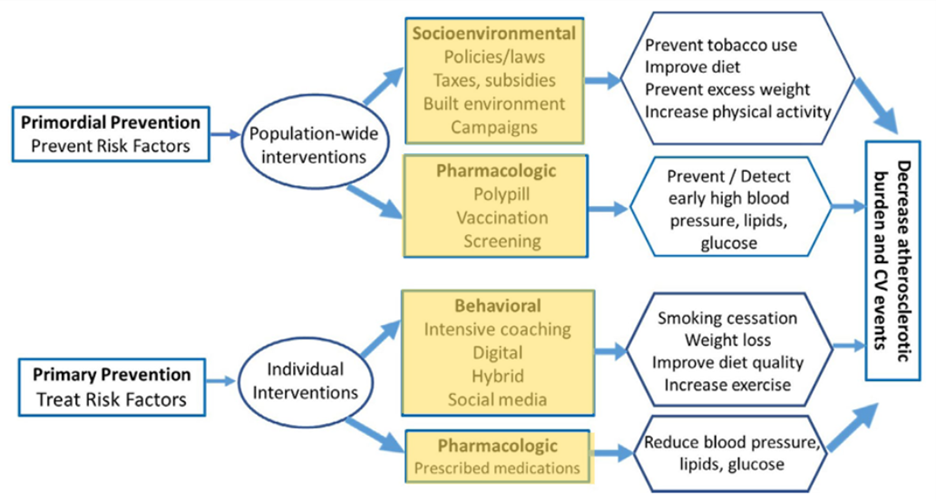
Considering the impact of therapeutic interventions on modifiable risk factors that lead to CVD, care providers can use no-code programs to curate personalized programs for every patient. The care programs developed for patients can consider individual biological risk factors and become highly specialized to monitor patients as needed.
Moreover, careful evaluation of family history and other risk factors can flag patients who are at risk. This will allow care providers to selectively focus their attention on individuals who need preventative care the most. Allocation of resources at the right opportunities will remove any hurdles in patients receiving appropriate care. (4)
Patient can not only undergo monitoring of their biological markers, but also lifestyle interventions such as introducing programs for quitting smoking, monitoring daily salt intake, etc. Apart from this, medication compliance can be monitored, and personalized coaching can be delivered, using social media and mHealth interventions.
Public health perspective
Given the worldwide impact of CVD on health, it is important to consider the public health perspective of the disease. It is evident that sustained reduction in disease burden cannot be achieved without reliable measurement and evaluation of surveillance data. Unfortunately in most low-income and middle-income countries, there is a lack of basic surveillance systems. (1)
Due to a lack of data, there also is a deficiency in prevention programs that cater to various populations.
How no-code can assist – population wide interventions:
No-code programs can be used by public health specialists to create surveillance programs with little to no efforts towards creating the digital software itself. The data gathered from these programs can be used to create effective laws and campaigns.
Moreover, these programs can be supplemented with education material based on latest research, that is freely available to patients and care providers. With no-code, programs can be constantly upgraded keeping up with the latest research.
Apart from surveillance programs, no-code can also be used to create screening programs that allow public health specialists to monitor the disease progression and risk factors of CVD by administering simple surveys occasionally.
The diagram below shows different risk factors that affect CVD, and which sectors no-code programs can be helpful in. (5)
Conclusion:
Low code is the new frontier of digital health that has the incredible potential to be highly personalized and dynamic. Diseases like cardiovascular problems require special investment from care providers and public health specialists equally. No-code can be a valuable resource for mHealth programs aimed at CVD prevention.
Bibliography:
- Franco M, Cooper RS, Bilal U, Fuster V. Challenges and Opportunities for Cardiovascular Disease Prevention. Am J Med. 2011 Feb 1;124(2):95–102.
- Kumar A. The impact of obesity on cardiovascular disease risk factor. Asian J Med Sci. 2018 Dec 12;10(1):1–12.
- The key issues in preventive cardiology – PubMed [Internet]. [cited 2022 Jul 29]. Available from: https://pubmed.ncbi.nlm.nih.gov/1345336/
- Crea F. Challenges in the prevention of cardiovascular diseases: traditional and non-traditional risk factors. Eur Heart J [Internet]. 2021 Jun 1 [cited 2022 Jul 29];42(21):2025–9. Available from: https://academic.oup.com/eurheartj/article/42/21/2025/6290946
- Gooding HC, Gidding SS, Moran AE, Redmond N, Allen NB, Bacha F, et al. Challenges and Opportunities for the Prevention and Treatment of Cardiovascular Disease Among Young Adults: Report From a National Heart, Lung, and Blood Institute Working Group. J Am Heart Assoc [Internet]. 2020 Oct 6 [cited 2022 Jul 29];9(19). Available from: https://pubmed.ncbi.nlm.nih.gov/32993438/
Insights
-

No-Code Tools for Managing Mental Health and Burnout in Healthcare Settings
Read more“P4” is a term that is often associated with future of medicine – prediction, prevention, personalization and patient participation. Many current health related technologies have already started moving towards the future and many more innovations are yet to come, that will make the goal of holistic medicine true.
-

Impact of health technology on diabetes management
Read more“P4” is a term that is often associated with future of medicine – prediction, prevention, personalization and patient participation. Many current health related technologies have already started moving towards the future and many more innovations are yet to come, that will make the goal of holistic medicine true.
